Emergency Services meeting - UK Parliament 2025
In May 2025, we organised a major event in the UK Houses of Parliament focusing on the Emergency Services (First Responder) community - the NHS, Fire & Rescue, Ambulance Service and Police.Our six excellent speakers addressed a full-house of around 170 people drawn mostly from the different services. Our panel of six amazing speakers:
- Steve Aumayer, CEO, East Sussex Healthcare NHS Trust
- Carl Dalby, Group Head of AI / Digital
- Nikki Watson QPM, Chief Fire Officer, Northamptonshire Fire and Rescue
- Rachael Swann, CEO, Grassroots Suicide Prevention
- Commander Richard Smith, Metropolitan Police Service
- Dr Saima Ajaz, Senior Clinical Lecturer, Lifestyle Medicine Physician, King’s College Hospital
Steve Aumayer
CEO, East Sussex Healthcare NHS Trust
 Steve talked about the different roles in his career to date and how helping people to realise their potential has been the common thread.
Steve talked about the different roles in his career to date and how helping people to realise their potential has been the common thread.
Factors affecting recruitment and retention of the workforce are multifactorial. An important thing for any organisation is having a clear mission – what we do and how people’s roles contribute. East Sussex has its challenges in terms of communications networks, but this means that we have a relatively stable workforce, as it is less easy to move around. From the Trust’s point of view, this is good, but it also means that we have an ageing workforce and all the challenges that this brings, including how to bring in younger people to build up ready to step into their shoes in due course.
The workplace is changing really quickly - right now. So, when we consider retaining people, we have to think about what people we will need with the current revolution taking place in working practices. The financial and productivity challenges and the introduction of automation and #AI to help us. What workforce do we actually need in the future? All we know is that it will probably be very different.
We will need a different set of skills to address a different way of working. Will we re-train the existing people? This could be a challenge, as training someone to work in community care takes time and we won’t have time with the pace of change. We need to address these questions and find solutions now.
So, the question is, what do we need and how are we going to build it?
Historically, we have seen organisations go under because they were complacent and relied too heavily on old business models. They failed to address the pace of change and innovate, they failed to address the needs of customers, and in the #NHS world, that is the needs of the population.
Whatever we do, these changes will happen – they already are happening.
We need to gain a deep understanding of what the future workforce will look like, what capabilities we will need, what we will need more of, less of and none of. Of course, that may mean that people need to be re-skilled so they can move on within or outside the organisation. We need to plan exit strategies for those leaving – the way we treat people will impinge on those remaining who will decide what sort of organisation you are running and whether they want to be part of it.
We need to paint a clear picture of what the organisation is, what it does, what its values are and what direction it is going. Engage people in the future and vision. We need to put in place a development plan now – if we wait, it will be too late. And, of course, do the obvious things – treat people with integrity, be kind and inclusive, look after people – we need to do the right thing as employers.
So, it is a holistic approach: join up the vision, strategy and goals with a clear plan to help people to realise their potential in an organisation where people want to stay and be part of achieving the goals. It’s about being a brilliant organisation, doing the right thing, looking after our people and the rest will follow.
Carl Dalby
Group Head of AI / Digital
 AI is everywhere today – it has been around for a very long time and it is increasingly important in most people’s lives.
AI is everywhere today – it has been around for a very long time and it is increasingly important in most people’s lives.
It is built into equipment (like SatNavs and mobiles) and now our favourite Search Engines give us ‘summaries’ when we search. We need to get used to it – if you’re not using it, then you can be replaced by someone who is. All the jobs today, tomorrow and thereafter are, and will be, AI augmented.
We are producing and giving access to our data on an unprecedented scale. We give away information about ourselves in exchange for the benefits it brings – using online mapping with GPS allows us to be tracked 24 hours a day. If you have an Alexa device, unless you switch it off, it is listening to you all the time. Using ‘free’ platforms like WhatsApp, Instagram and all the others gives away our data – it is a currency and has value.
Robots are replacing humans in hazardous situations and reducing risk and even saving lives – like in Fire & Rescue. We even have robot vacuum cleaners and lawn mowers.
We can now chat to data – like we do to a person, but actually to the data through AI. It is like an entity in itself, a new colleague.
This is the ‘now’ (if we can afford to have the access) and ‘tomorrow’ will bring more.
We now have access to virtually every book written from our devices, for example. We are using it in our work lives increasingly and it is the future. AI to help with diagnosis of breast tumours from mammograms, for example. AI to answer questions. AI to bring new questions to consider.
Healthcare is one of the areas in which AI will have a major impact. ‘Custom’ healthcare is already here and will be the thing of the future. AI will help create personalised #medicine.
The Emergency Services need to work out how to access the plethora of data to enhance the work they do. To use them to help protect us. This is the future.
Nikki Watson QPM
Chief Fire Officer, Northamptonshire Fire and Rescue
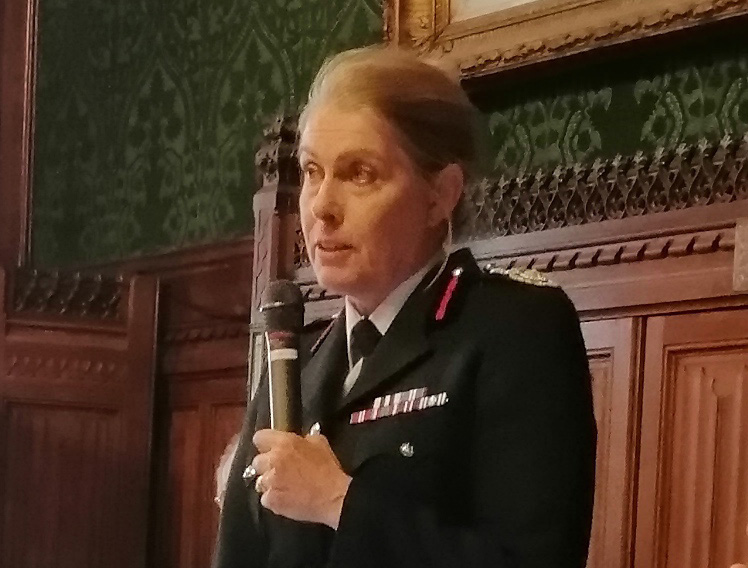 The Emergency Services are exactly that – services. Most of the budget is spent on staff salaries, preventing risk and protecting the public from fire, road traffic collisions and other emergencies. It regularly exposes Firefighters to traumatic incidents, as well as a variety of contaminants which can present serious health risks.
The Emergency Services are exactly that – services. Most of the budget is spent on staff salaries, preventing risk and protecting the public from fire, road traffic collisions and other emergencies. It regularly exposes Firefighters to traumatic incidents, as well as a variety of contaminants which can present serious health risks.
The challenge is to have the resources and resilience to respond to emergencies in every inch of the UK in a timely manner. Budgets are contracting and the #health and #wellbeing of staff have to be protected so they can respond quickly when the public needs.
Climate change is causing more wildfires and increased flooding. The FRS is working to mitigate these emerging risks. Unknown to most, flooding is not within the statutory remit, but, despite that, the public expects it to respond, and we do.
The response to new risks, exposure to various contaminants and the usual risks from fires, are the subject of continual development within the Service. This includes improved working practices and personal protective equipment.
The Service has a ‘male’ culture due to the physicality of the work. This can mean that people are reluctant to seek help and support. Working collaboratively with the other Services is an important approach to addressing this challenge.
A happy, healthy, motivated and well-led workforce which is productive, effective and efficient is critical for keeping our community safe. Wellbeing is a holistic concept, including mental, physical and spiritual wellness – feeling good and functioning well. Within FRS, wellbeing has traditionally been defined and delivered at the local level. It was not sector-focused with evidence-based delivery and did not address the variety of needs for different roles.
FRS has traditionally worked closely with #Police colleagues and we share Oscar Kilo UK, but the needs of Firefighters are different and the National Fire Chiefs Council and Fire Fighters Charity have been working with Nottingham Trent University to research the needs of the workforce. From this, a national framework and toolkit are being developed to help at the local level.
Investing in services should be straightforward when the organisation prioritises health and wellbeing and provides the investment. Collaboration with partners, public and private, to understand the needs and to provide the required interventions will deliver the results. Investment is critical to enable the Services to deliver to, and protect, the community.
Rachael Swann
CEO, Grassroots Suicide Prevention
 In the UK, 17 people per day die by suicide. Of those 17, five are in contact with mental health services and four of those are assessed as low- or no-risk.
In the UK, 17 people per day die by suicide. Of those 17, five are in contact with mental health services and four of those are assessed as low- or no-risk.
Contact Grassroots Suicide Prevention if you or anyone around you could benefit from help or support.
A person-centred approach is very effective in suicide prevention. One in five of us will have suicidal thoughts and one in 15 will actually attempt suicide during their lifetime.
The Stay Alive App (see below) is recommended by the NHS. It has been available since 2014 and there have been over 900,000 downloads. It is free. It is confidential and it contains no adverts. Recently, the number of downloads has been increasing, which indicates that people are looking for help and support. The App is aimed at anyone who is struggling themselves, or if they're supporting someone else. Over a quarter of users have reported that it helps them stay safe and alive.
First Hand is another important resource. It is for people who have witnessed suicide when they didn’t know the person. People like Emergency Responders who face this during their work, or even people who just happened to be there. It is a guide to help support the person over the first few days, then the coming weeks and moving on from there.
The Grassroots Suicide web site also has a wealth of information, help and support. There are podcasts from people with lived experience and information from professionals to allow people to take a deeper dive. There is also information about causes, warning signs and, of course, stories of recovery.
Commander Richard Smith
Metropolitan Police Service
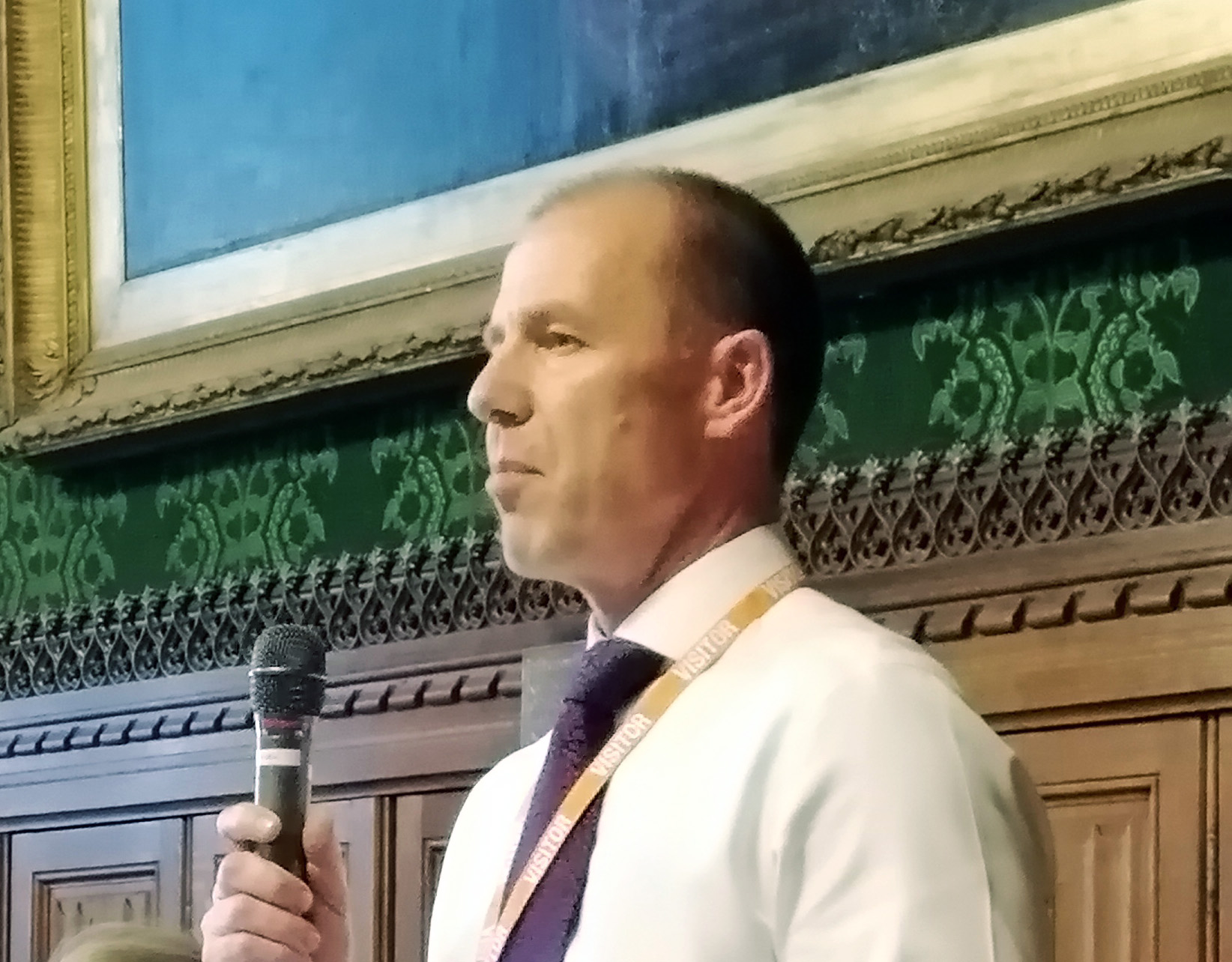 Good leadership has always been critical to every organisation and, with the challenges faced in society, the economic situation, demographic and many other changes, it could be argued that today is even more of a challenge.
Good leadership has always been critical to every organisation and, with the challenges faced in society, the economic situation, demographic and many other changes, it could be argued that today is even more of a challenge.
Richard looked at leadership though a Policing lens. There is a public expectation of the Police and, alongside that, we have to consider how expectation is met which often exposes Officers to risk.
Policing is a people business – the most valuable asset is genuinely the people. Their job is to protect the public, often during the most challenging times of their lives. This exposes staff to traumatic incidents on a very regular basis and that often puts them in harms way.
Police officers face trauma throughout their careers. This may be during really big incidents like 7/7 and terrorist attacks, but alongside that, there are repeated exposures to lower-profile ones. These include road traffic accidents, assaults, murder scenes, rape and child abuse, so it isn’t just the high-profile ones that contribute to their trauma.
Many Officers also face day-to-day aggression, abuse, hostility, possible physical threat, being spat at and, no matter how well trained they are, these things have an impact. A Police Officer is assaulted roughly every 10 minutes (that’s 50,000 per year) in this country and the chance is higher in the first five years of service – and that stays with them for life. Being assaulted used to be considered to be part of the job. Being assaulted should never be part of anybody’s job. There is an initiative called Operation Hampshire which encourages Officers to report incidents and to try to ensure that they get the best possible support.
It is not all physical trauma, either. Police Officers also have to view, often horrific, material online such as child sexual abuse and harm, terrorist incidents and beheading videos as part of their work. Officers are humans, and this sort of thing traumatises them in their work to keep the public safe and free from harm.
Oscar Kilo (a Police support organisation) estimates that one in five Officers will suffer from Post Traumatic Stress (PTSD).
On top of all this, there is the absolutely-necessary accountability that Officers face. Officers are required to use force in the line of duty and, sometimes, that even includes lethal force. Whilst the scrutiny is right, it does come with a cost and also media and public responses. The scrutiny has to be handled properly and fairly and with compassion to all involved.
The work of the Police is often not conducive to family and social life. Many Officers are partners, parents and carers and this further adds to their challenges and stress. Officers and their families face online trolling and abuse, on top of everything else. The demand for Policing is 24 / 7 / 365 and the organisation needs to take these things into account. Shift work adds to the challenges and makes it more difficult for people to look after their wellbeing, nutrition and fitness.
The role of the leader is critical in all this. In Australia, there has been some work around ‘healthy leadership’ – making it OK to say that you are not OK and to admit that you have problems. The culture here is still ‘grin and bear it’ and leaders have to lead by example if change is to happen.
Officers go to work for a reason – their mission. And that is about keeping the public safe. We need to respect that and do all possible to support them in this critical role.
Dr Saima Ajaz
Senior Clinical Lecturer, Lifestyle Medicine Physician, King's College Hospital
 There is an increasing appreciation about the importance of sustaining a healthy lifestyle, a healthy nation and being able to prevent disease.
There is an increasing appreciation about the importance of sustaining a healthy lifestyle, a healthy nation and being able to prevent disease.
Saima talked about her research, her work as a Specialist Hepatologist at King's College Hospital NHS Foundation Trust and how it indicates that many problems can be avoided. She asked the packed audience how they want to be at the age of 80. The conclusion: full of life, able to look after themselves and active.
It is important to move from the current system that focuses on the treatment of illness to one of prevention. Saima quoted Desmond Tutu, "There comes a point when we have to stop just pulling people out of the river. We need to go upstream and find out why they’re falling in".
'Future medicine' will be a matter of tailored treatment, finding the root causes, predicting and preventing. Things like #AI will have their role – analysing huge amounts of data and finding new questions and answers.
Liver disease is the third major cause of premature death. 90% of liver disease can be prevented. 25 to 38% of the global population suffers from ‘fatty liver disease’ (MASLD). In a study carried out in South London, over 50% of the people taking part had fatty liver disease (and had no idea) and 26% had advanced liver disease (fibrosis). The average BMI was 32 kg/m2 which is regarded as borderline ‘obese’ medically – and, remember, it is the average of the group. Only 48% of the whole group considered themselves ‘overweight’. When they were made aware of the potential problems the future may hold, almost all expressed a keen interest in learning about lifestyle modifications that could help. This shows that, when people are made aware, they are willing to do something about it.
How do we achieve a raised awareness? We cannot screen the whole population, so lifestyle strategies have to be part of our care. Sadly, there is no funding for this work. There is funding for ‘cure’, but not ‘prevention’.
Saima started her own 'LIVFIT' project in 2019 and ran meetings with experts every few months to raise awareness and education in the local population. This resulted in 85-95% of people achieving weight loss of 5-10% body weight and 5% showed significant improvement in clinical factors. This proves that it really works and there are clear benefits, both to the patients, and to the healthcare system. Fifty patient advocates have now been trained to go into their communities to spread the word.
We cannot solve the problems with the same thinking that created them in the first place. We have to take a new, wider view, whether it is lifestyle education or AI. It will take effort, but educating and empowering patients is a proven route to success.
© R2 Potential CIC 2013-2026